Ozempic Risk Assessment Tool
Patient Risk Assessment
Risk Assessment Results
Critical Actions
Recommendations
When a patient walks into a weight‑loss clinic, the buzzword on most consultation forms is Ozempic. Ozempic is a brand‑name GLP‑1 receptor agonist (semaglutide) originally approved for type 2 diabetes but now widely prescribed to jump‑start weight loss. While the drug can shave off 10-15 % of body weight in a few months, every medication carries trade‑offs. Below we break down the most common-and sometimes surprising-downside of Ozempic so you can weigh the benefits against the risks.
Why Ozempic Became a Weight‑Loss Favorite
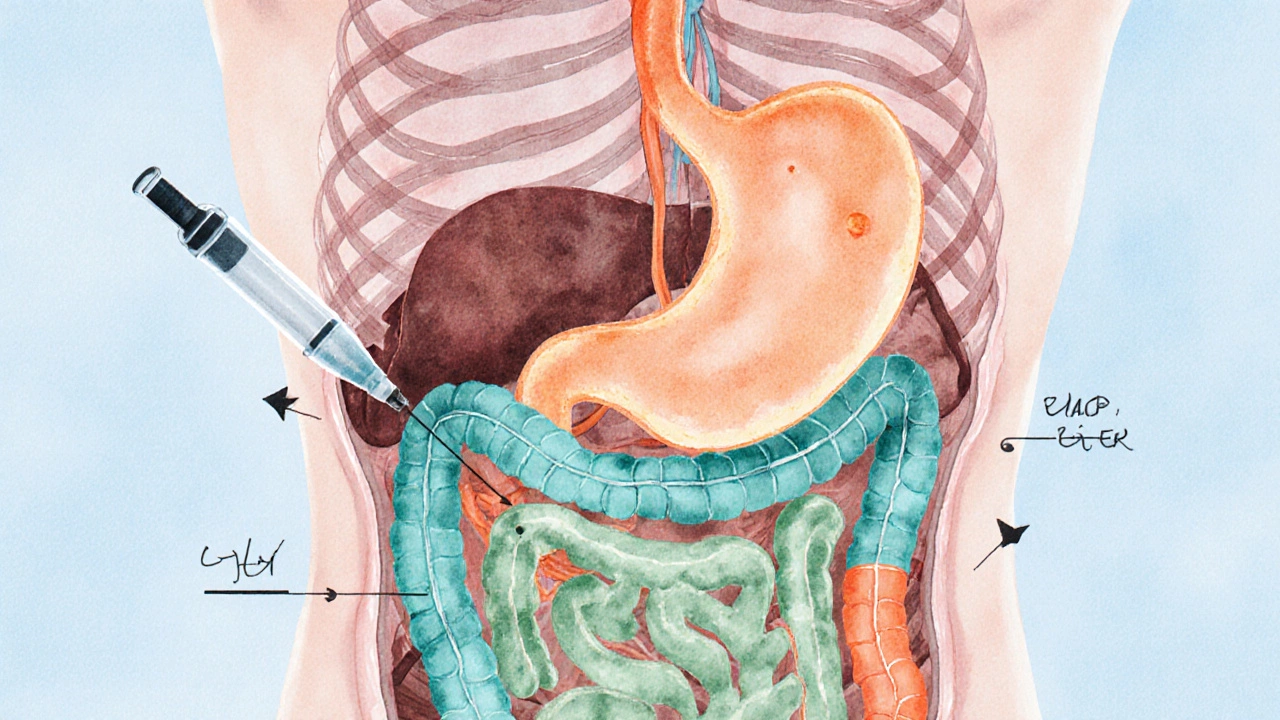
GLP‑1 agonists mimic a gut hormone that tells the brain you’ve eaten, slowing gastric emptying and curbing appetite. In clinical trials, patients on semaglutide lost an average of 12 % of total body weight, outperforming most diet‑only programs. That potency, combined with once‑weekly injections, made Ozempic a go‑to prescription in many clinics.
Common Side Effects You’ll See on the Front‑Line
- Nausea and vomiting - Reported by up to 30 % of users, usually mild to moderate and often subsides after the first few weeks.
- Diarrhea or constipation - Gut motility changes can swing either way; around 15 % experience one or the other.
- Headache - A frequent complaint, typically linked to dehydration from gastrointestinal upset.
Most of these issues are dose‑dependent. Starting at a low dose (0.25 mg weekly) and titrating up helps many patients stay on the drug.
Serious but Rare Risks
Beyond the everyday aches, clinicians must keep an eye on less common but potentially dangerous events.
- Pancreatitis - Inflammation of the pancreas occurs in roughly 0.1 % of patients. Look for severe upper‑abdominal pain that radiates to the back.
- Gallbladder disease - Rapid weight loss can precipitate gallstones. Ultrasound screening is advised if patients develop right‑upper‑quadrant pain.
- Thyroid C‑cell tumors - Animal studies showed a link, and the FDA requires a black‑box warning. Family history of medullary thyroid carcinoma should be a contraindication.
- Kidney function decline - Dehydration from vomiting can precipitate acute kidney injury, especially in older adults.
These events are uncommon, but early detection can prevent complications. Document any abdominal pain, persistent nausea, or changes in urine output promptly.
Impact on Blood Sugar and Diabetes Management
For patients with type 2 diabetes, Ozempic often improves HbA1c by 1-2 %. However, the glucose‑lowering effect can overshoot in non‑diabetic users, leading to hypoglycemia if combined with other glucose‑lowering agents. In a weight‑loss clinic, be cautious when the patient is also on insulin or sulfonylureas; dose adjustments are typically required.
Cost, Insurance, and Accessibility
Unlike generic metformin, Ozempic carries a premium price tag-about $900-$1,200 per month in the U.S. In India, the cost is lower but still a significant out‑of‑pocket expense for many patients. Insurance coverage varies; most plans still classify it under diabetes, not weight loss, which can limit reimbursements. Clinics should counsel patients on financial assistance programs offered by the manufacturer.
Long‑Term Sustainability and Weight Regain
Studies tracking patients for two years show that once the injection stops, many regain 30-40 % of the lost weight. This rebound isn’t unique to Ozempic-any pharmacologic weight‑loss aid tends to require ongoing therapy for maintenance. Counsel patients that the drug is a tool, not a magic bullet; lifestyle changes remain essential.
Practical Checklist for Clinicians
| Aspect | What to Watch For | Action |
|---|---|---|
| Gastro‑intestinal | Nausea, vomiting, diarrhea | Start low, hydrate, consider anti‑emetics |
| Pancreas | Severe abdominal pain, elevated lipase | Discontinue, refer to gastroenterology |
| Thyroid | Family history of medullary thyroid carcinoma | Contraindicate use, screen with calcitonin if uncertain |
| Kidneys | Dehydration, rising creatinine | Monitor labs, adjust dose, ensure fluid intake |
| Cost | Insurance denial, high out‑of‑pocket | Discuss assistance programs, explore alternatives |

How to Discuss Risks with Patients
Clear communication builds trust. Use the "benefit‑risk" format: "You could lose up to 15 % of your weight, but there’s a 1‑in‑1,000 chance of pancreatitis. Here’s how we’ll watch for it." Provide printed handouts summarising side‑effects, and schedule a follow‑up after the first four weeks to assess tolerance.
Alternative Options When Ozempic Isn’t Right
- Other GLP‑1 agonists - Tirzepatide (Mounjaro) offers similar weight loss with a slightly different side‑effect profile.
- Oral agents - Metformin can aid modest weight loss with a well‑known safety record.
- Non‑pharmacologic programs - Structured diet, behavior therapy, and bariatric surgery for severe obesity.
Choosing an alternative depends on the patient’s medical history, budget, and willingness to inject weekly.
Bottom Line
Ozempic delivers impressive weight‑loss results, but the downsides-gastro‑intestinal upset, rare pancreatitis, potential thyroid concerns, and high cost-require diligent screening and monitoring. Weight‑loss clinics that pair the drug with robust lifestyle coaching and transparent risk discussion can harness its benefits while minimizing harm.
Can I take Ozempic if I don’t have diabetes?
Yes. Ozempic is FDA‑approved for chronic weight management in adults with a BMI ≥ 30 kg/m² or BMI ≥ 27 kg/m² with at least one weight‑related condition, even if you’re not diabetic. However, doctors still need to assess your overall health before prescribing.
How long does it take to see weight loss?
Most patients notice a reduction in appetite within the first two weeks. Clinically significant weight loss (5 % of body weight) typically appears after 8-12 weeks of consistent dosing.
What should I do if I experience severe nausea?
Talk to your clinician immediately. They may reduce the dose, split the injection schedule, or prescribe an anti‑nausea medication. Staying hydrated and eating small, bland meals can also help.
Is Ozempic safe for pregnant or breastfeeding women?
Current data are limited, and the drug carries a pregnancy warning. It’s generally advised to avoid Ozempic during pregnancy and lactation unless the benefits clearly outweigh the risks.
Will I need to continue Ozempic forever?
Weight maintenance usually requires ongoing therapy. If you stop, most patients regain a portion of the weight lost, so a long‑term plan-whether continued Ozempic, a switch to another agent, or intensified lifestyle changes-is essential.