Dental Implant Eligibility Calculator
How Your Factors Impact Implant Success
This tool helps you understand your personal eligibility for dental implants based on key factors discussed in the article. Results are for informational purposes only and not medical advice.
When you think about restoring missing teeth, Dental implants are often the first solution that comes to mind. They feel permanent, look natural, and help keep the jawbone healthy. But many wonder if there’s a deadline- a point when the jaw simply won’t support an implant anymore. This guide breaks down the key factors that determine whether it’s truly too late, from age and bone health to medical conditions and lifestyle choices. By the end, you’ll know the red‑flags, the work‑arounds, and the steps you can take to improve your chances.
Why Timing Matters
Implant success hinges on a process called osteointegration-the direct bond between the titanium post and the jawbone. This fusion requires sufficient bone volume and density. As we age, bone naturally remodels and can lose density, especially after a tooth is lost. The longer a gap stays empty, the more the surrounding bone can resorb, making the site less ideal for an implant.
Age Is Not the Only Clock
While there’s no strict age limit, certain age‑related trends affect eligibility:
- Young adults (under 18): Their jaws are still growing, so placing a permanent fixture can lead to misalignment later.
- Older adults (65+): Bone density tends to decline, and conditions like osteoporosis become more common, increasing the risk of implant failure.
- Middle‑aged patients (30‑60): Generally have the best balance of bone quality and healing potential, but lifestyle factors can tip the scale.
Age alone isn’t a deal‑breaker; it’s how age interacts with health and oral conditions that matters.
Medical Conditions That Can Delay or Block Implants
Several health issues directly influence implant viability:
- Periodontitis - Advanced gum disease destroys the supporting bone. Untreated, it can make the implant site unstable.
- Diabetes - Poorly controlled blood sugar slows healing and raises infection risk.
- Smoking - Nicotine constricts blood vessels, impeding bone growth and increasing failure rates.
- Osteoporosis - Reduces overall bone density, making the jaw less able to hold an implant.
Managing these conditions-through proper medication, lifestyle changes, and dental care-can shift the odds back in your favor.

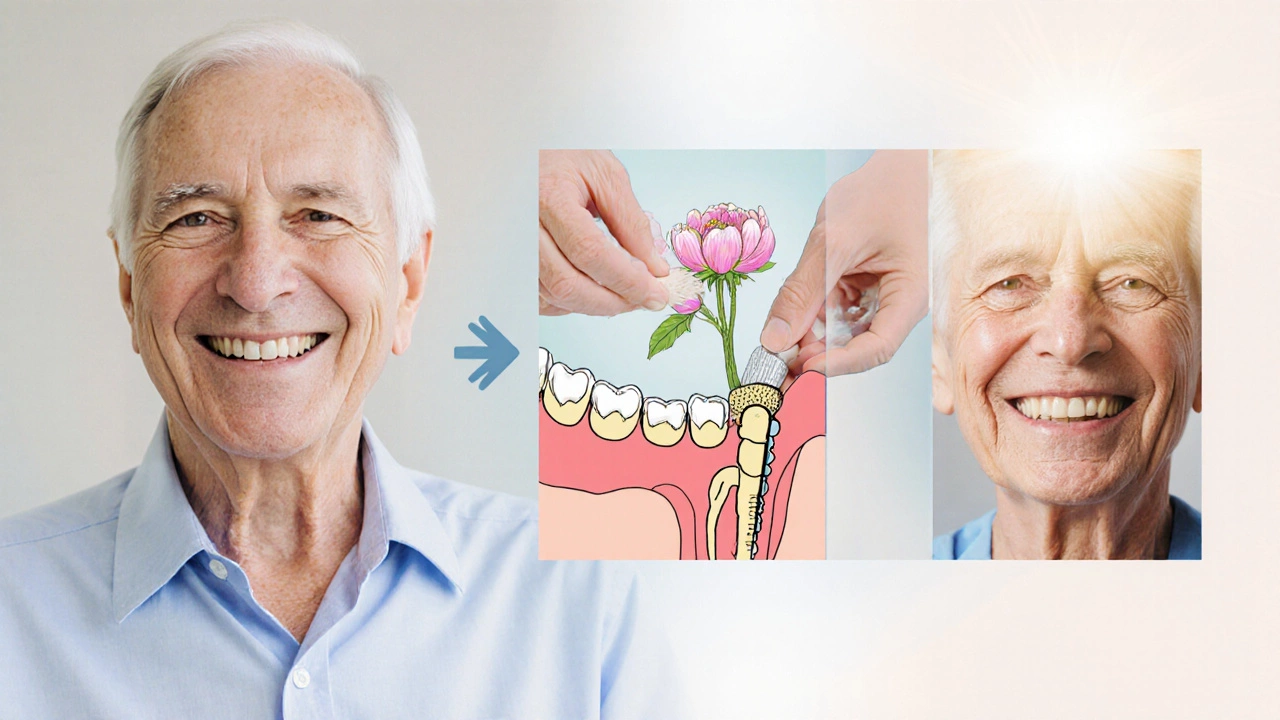
Bone Health & The Role of Bone graft
If the jawbone is too thin or has holes where a tooth used to be, a bone graft can rebuild the foundation. There are three main types:
- Autograft - bone taken from another area of the patient’s own body.
- Allograft - donated human bone processed to remove cells.
- Synthetic graft - materials like hydroxyapatite that act as a scaffold.
Grafts typically need 3‑6 months to fuse, after which the site can be evaluated for dental implants. In many cases, a well‑executed graft turns a “too late” scenario into a viable one.
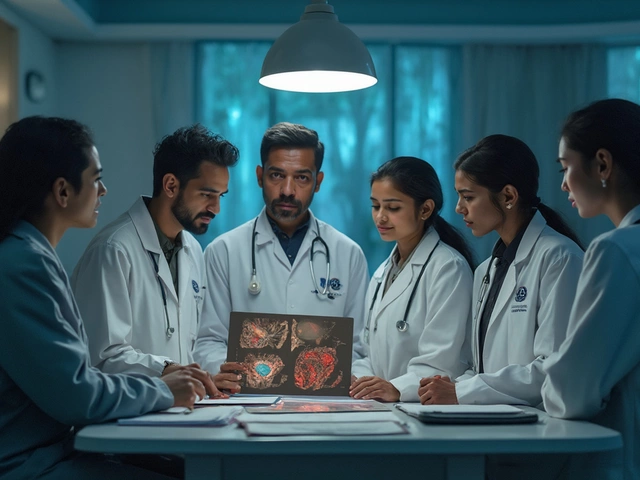
How Dentists Assess Readiness
Before any surgery, a comprehensive evaluation is performed:
- Clinical exam: Checks gum health, plaque levels, and any signs of infection.
- Imaging: Cone‑beam CT scans give a 3‑D view of bone volume and density (often reported as Hounsfield Units).
- Bone density measurement: The Jawbone density reading helps predict how well the implant will integrate.
- Medical history review: Looks for diabetes, osteoporosis, medications that affect bone turnover (e.g., bisphosphonates).
- Implant stability quotient (ISQ): For existing implants, this numeric value gauges how firmly the implant is anchored; a low ISQ may suggest a need for additional bone augmentation.
Based on this data, the clinician decides whether to place a standard implant, recommend a graft, or explore alternative prosthetics.
When Traditional Implants Aren’t Feasible
If after evaluation the jawbone is still insufficient, or if health factors make surgery risky, there are proven alternatives:
| Option | Typical Cost (US$) | Procedure Time | Longevity | Maintenance |
|---|---|---|---|---|
| Dental implants | 3,000-6,000 per tooth | 2‑3 visits over 4‑6 months | 10‑25+ years | Regular brushing, occasional check‑ups |
| Fixed bridge | 1,000-2,500 per unit | 1‑2 visits over 2‑3 weeks | 5‑15 years | More plaque traps; may need replacement |
| Removable denture | 500-1,500 | 1‑2 visits | 3‑10 years | Daily cleaning; adhesive use |
For patients with limited bone, techniques like All‑on‑4-where four strategically placed implants support an entire arch-can reduce the amount of graft needed. Even mini dental implants, which are thinner and require less bone, serve as stabilizers for overdentures.
Boosting Your Chances: Practical Steps
Even if you’re borderline, a few lifestyle tweaks can tip the balance:
- Quit smoking at least 2‑4 weeks before surgery.
- Maintain strict oral hygiene: brush twice daily, floss, and use antimicrobial mouthwash.
- Manage chronic conditions-keep diabetes HbA1c below 7% and ensure osteoporosis meds are optimized.
- Eat bone‑friendly foods rich in calcium, vitamin D, and protein.
- Consider pre‑operative vitamin D supplementation if you’re deficient.
These actions improve healing, reduce infection risk, and often increase bone density enough to make an implant possible.
Key Takeaways
- There’s no universal “cut‑off age”; bone health, not age, is the real limiter.
- Conditions like periodontitis, uncontrolled diabetes, smoking, and osteoporosis can delay or prevent implants.
- Bone loss after tooth loss is reversible with grafts or alternative implant designs.
- Comprehensive evaluation-clinical exam, CT scan, and health review-determines eligibility.
- If standard implants aren’t viable, bridges, dentures, All‑on‑4, or mini implants offer effective solutions.
Frequently Asked Questions
Can seniors get dental implants?
Yes, many seniors succeed with implants if their jawbone is healthy and they manage any chronic conditions. Bone grafts or All‑on‑4 can address reduced bone density.
How long does a bone graft take to heal?
Typically 3‑6 months, depending on graft material and the patient’s healing capacity.
Will smoking ruin my implant?
Smoking significantly raises failure rates. Quitting several weeks before and after surgery improves success chances dramatically.
Is a mini dental implant as strong as a regular one?
Mini implants have smaller diameters, making them suitable for thinner bone or overdentures. They’re sturdy for those uses, though they’re not ideal for supporting large single crowns.
What’s the success rate for implants in older adults?
When bone quality is adequate, success rates hover around 95% even in patients over 70. The key is thorough evaluation and managing health factors.
Bottom line: It’s rarely a matter of “too late” in the absolute sense. Rather, it’s about whether the underlying bone and health conditions are ready for a permanent fixture. With proper assessment, possible bone augmentation, and healthy lifestyle choices, most people can find a viable path to a restored smile.