IVF Recovery Timeline Calculator
How Soon Can You Start IVF After Having a Baby?
Get personalized guidance based on medical guidelines from major journals and clinical experience
Your Personalized IVF Timeline
Recommended Waiting Period
Key Factors Affecting Your Timeline
Next Steps
Getting pregnant again after having a baby doesn’t always happen naturally-and if you’re considering IVF, timing matters. Many couples wonder: how soon is safe? How soon is smart? And what does your body actually need to recover? There’s no one-size-fits-all answer, but understanding the medical guidelines, your physical recovery, and your emotional readiness can help you make the right call.
Medical Guidelines: What Doctors Recommend
Most fertility specialists and obstetricians suggest waiting at least 18 to 24 months after giving birth before starting another IVF cycle. This isn’t just a suggestion-it’s based on data from large studies, including those published in the British Medical Journal and the American Journal of Obstetrics and Gynecology. These studies show that conceiving too soon after delivery increases risks for both mother and baby, including preterm birth, low birth weight, and placental problems.
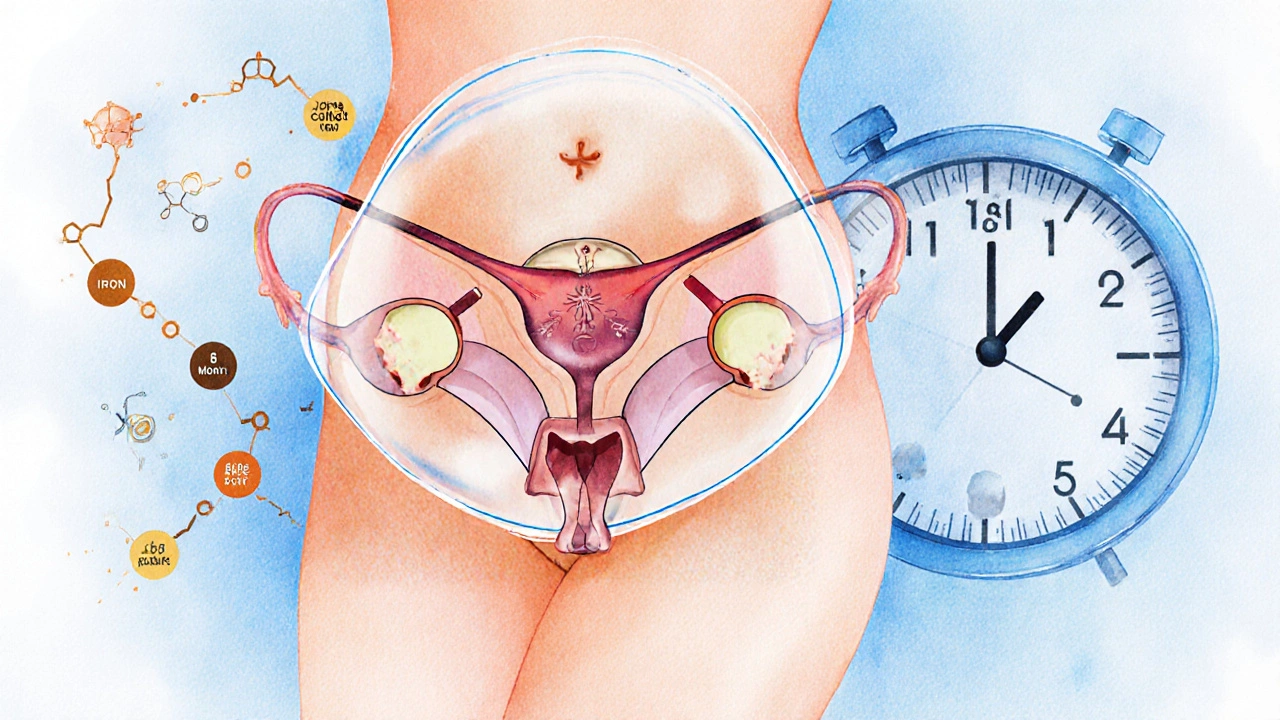
Why 18 to 24 months? Your body needs time to rebuild its nutrient stores, especially iron and folate, which are heavily depleted during pregnancy and breastfeeding. Your uterus also needs to fully heal from the stretch and strain of carrying a baby. Even if you had a C-section, internal scar tissue needs to mature before another pregnancy can safely begin.
What If You’re Under 35 and Want to Move Faster?
Age plays a big role. If you’re under 35 and your fertility hasn’t been affected by previous treatments, some clinics may consider starting IVF as early as 6 months after delivery-if you’re not breastfeeding and your menstrual cycle has returned to normal. But this is rare and only done after thorough evaluation.
One 32-year-old patient I worked with started IVF at 7 months postpartum. She had a healthy vaginal delivery, stopped breastfeeding at 4 months, and her hormone levels were back to baseline. Her doctor approved it because she had no complications and was emotionally ready. But her embryo transfer was delayed by two months because her uterine lining was too thin. That’s not uncommon.
Breastfeeding and IVF: Can You Do Both?
Breastfeeding suppresses ovulation through high prolactin levels. That’s why many women don’t get their period back right away. But once you stop breastfeeding, your hormones start shifting again. Most women resume regular cycles within 2 to 6 months after weaning.
Starting IVF while still breastfeeding isn’t recommended. Fertility drugs like gonadotropins can pass into breast milk, and there’s not enough safety data to say it’s harmless. Plus, the stress of IVF-daily injections, appointments, emotional ups and downs-can interfere with milk supply and your ability to care for your newborn.
If you’re still nursing and want to start IVF, plan to wean first. Work with your doctor to monitor your hormone levels and track ovulation with blood tests or ovulation predictor kits. Don’t assume your period returning means you’re ready. Your body might be ovulating, but your uterine lining could still be thin or your progesterone too low.
Physical Recovery: More Than Just Your Uterus
Your body doesn’t just recover after childbirth-it rebuilds. Your pelvic floor muscles may still be weak. Your core might not be fully reconnected. Hormones like cortisol and thyroid can stay out of balance for months, especially if you’re sleep-deprived or stressed.
IVF requires a strong foundation. If you’re running on empty, your body may not respond well to stimulation drugs. Studies show that women with low BMI, high stress, or poor sleep quality have lower egg retrieval numbers and poorer embryo quality.
Before starting IVF, get a full blood panel: iron, vitamin D, thyroid, and AMH. Check your BMI. If you’re under 18 or over 29, your chances of success drop. If your iron is low, fix it first. If your vitamin D is under 40 ng/mL, start supplementing. These aren’t optional steps-they’re part of the protocol.
Emotional Readiness: The Hidden Factor
Having a baby changes everything. If your first child was hard to conceive, you might feel pressure to get pregnant again fast. Or maybe you’re grieving the loss of your pre-baby life and aren’t emotionally ready to go through IVF again.
It’s okay to feel overwhelmed. Many women report anxiety, guilt, or exhaustion when thinking about another round of IVF. One study from the Journal of Psychosomatic Obstetrics & Gynecology found that women who started IVF within 12 months of childbirth had higher rates of depression and treatment dropout.
Ask yourself: Are you doing this because you want to, or because you feel you have to? Talk to a counselor who specializes in fertility. Join a support group for parents who’ve had IVF. You’re not alone-and your mental health matters as much as your physical health.
What About After a Miscarriage or Stillbirth?
If your last pregnancy ended in loss, the timeline changes. Some doctors recommend waiting one full menstrual cycle before starting IVF again. Others suggest waiting 3 to 6 months to allow for emotional healing.
There’s no evidence that waiting longer improves success rates after a miscarriage-but emotional readiness does. If you’re not ready to go through injections, scans, and hope again, it’s okay to wait. There’s no rush. Your grief isn’t a delay-it’s part of your journey.

Real-World Examples: When People Got It Right
Emma, 34, had her first child at 31 via IVF. She waited 22 months after delivery. She weaned her baby at 10 months, got her period back at 14 months, and started IVF at 20 months. Her first transfer after waiting worked. She’s now the mom of two healthy kids.
Mark and Lisa, 38 and 36, started IVF at 9 months postpartum after a C-section. They didn’t breastfeed. But their first cycle failed because Lisa’s ovaries didn’t respond well. Turns out, her progesterone was low and her thyroid was underactive. After fixing those issues and waiting another 6 months, their second cycle succeeded.
These stories show the same thing: timing isn’t just about months. It’s about your body, your health, and your readiness.
When to See a Fertility Specialist
You don’t have to wait until you’re ready to start IVF to get advice. If you’re planning another pregnancy, see a fertility specialist 3 to 6 months before you want to begin. They can:
- Check your ovarian reserve with an AMH test
- Assess your uterine health with a saline ultrasound
- Test for thyroid or autoimmune issues that affect fertility
- Review your previous IVF cycle and adjust your protocol
Even if you’re not ready yet, this gives you a baseline. You’ll know what to work on before you start.
Bottom Line: Patience Pays Off
Waiting 18 to 24 months after having a baby before starting IVF is the safest, most effective path. It gives your body time to heal, your hormones time to reset, and your mind time to breathe. Rushing can lead to failed cycles, complications, or burnout.
That doesn’t mean you have to wait blindly. Use the time wisely: get your labs done, fix nutrient gaps, work on your mental health, and build a support system. When you do start IVF, you’ll be stronger, healthier, and better prepared.
Your next child deserves that. So do you.
Can you get pregnant naturally after having a baby and before starting IVF?
Yes, it’s possible. Many women ovulate and conceive naturally after childbirth, especially if they’re not breastfeeding. But if you’ve struggled with fertility before, don’t assume your body will bounce back easily. Track your cycles with ovulation tests or basal body temperature. If you’re not pregnant after 6 to 12 months of trying, see a fertility specialist-don’t wait until you’re ready for IVF.
Does breastfeeding delay IVF success?
Breastfeeding itself doesn’t make IVF less successful-it just delays it. High prolactin from nursing suppresses ovulation and lowers estrogen, which affects egg development and uterine lining. Once you wean, your body usually returns to normal within a few months. Starting IVF while still breastfeeding isn’t advised due to unknown effects on milk supply and baby safety.
Is it safe to do IVF after a C-section?
Yes, but timing matters. Most doctors recommend waiting at least 18 months after a C-section before another pregnancy. This gives the uterine scar time to heal properly. Starting IVF too soon increases the risk of uterine rupture during pregnancy. Your doctor will likely do a follow-up ultrasound to check scar thickness before you proceed.
How long does it take for periods to return after childbirth?
It varies. If you’re not breastfeeding, your period usually returns within 6 to 12 weeks. If you’re breastfeeding, it can take 3 to 12 months-or longer. The return of your period doesn’t mean you’re fertile yet. Ovulation can happen before your first period, so track it with tests or basal body temperature if you’re trying to conceive.
Should I wait longer if I had complications during delivery?
Absolutely. If you had preeclampsia, postpartum hemorrhage, gestational diabetes, or a prolonged hospital stay, your body needs more time to recover. Talk to your OB-GYN and fertility specialist. You may need extra testing for blood pressure, kidney function, or insulin resistance before starting IVF. Rushing could put your health-and future pregnancy-at risk.
Can stress affect IVF success after having a baby?
Yes. Chronic stress raises cortisol, which can disrupt ovulation, lower egg quality, and reduce uterine blood flow. After having a baby, stress from sleep deprivation, parenting demands, or emotional exhaustion can make IVF harder. Managing stress through therapy, sleep routines, or mindfulness practices can improve your chances as much as any medication.






