Ever wondered which operation sits at number five on the orthopedic surgery popularity list? It’s not a hip or knee replacement - it’s a rotator cuff repair. Below we break down why this shoulder procedure ranks fifth, what it involves, and how it stacks up against the other top surgeries.
Quick Takeaways
- The 5th most common orthopedic surgery in the United States is rotator cuff repair.
- It follows total knee replacement, total hip replacement, lumbar spinal fusion, and knee arthroscopy.
- Typical patients are adults 50‑70 years old with shoulder pain or loss of function.
- Recovery averages 4‑6 months, with physical therapy essential for a good outcome.
- Average hospital charge runs around $15,000‑$20,000, varying by technique and region.
How Orthopedic Procedure Rankings Are Determined
Hospitals and insurance databases track the volume of each surgical code (CPT). By aggregating data from the National Inpatient Sample and outpatient surgery centers, analysts can rank procedures by annual case count. The top five consistently appear in the same order because they address the most common age‑related joint problems: knee osteoarthritis, hip degeneration, spinal disc disease, meniscal tears, and shoulder tendon tears.
Overview of the Top Five Orthopedic Surgeries
| Rank | Procedure | Typical Patient Age | Average Recovery Time | Average Cost (USD) |
|---|---|---|---|---|
| 1 | Total Knee Replacement | 60‑75 | 3‑6 months | $30,000‑$45,000 |
| 2 | Total Hip Replacement | 55‑70 | 2‑4 months | $28,000‑$40,000 |
| 3 | Lumbar Spinal Fusion | 45‑70 | 4‑12 months | $45,000‑$60,000 |
| 4 | Knee Arthroscopy (including meniscectomy) | 30‑55 | 2‑8 weeks | $8,000‑$12,000 |
| 5 | Rotator Cuff Repair | 50‑70 | 4‑6 months | $15,000‑$20,000 |
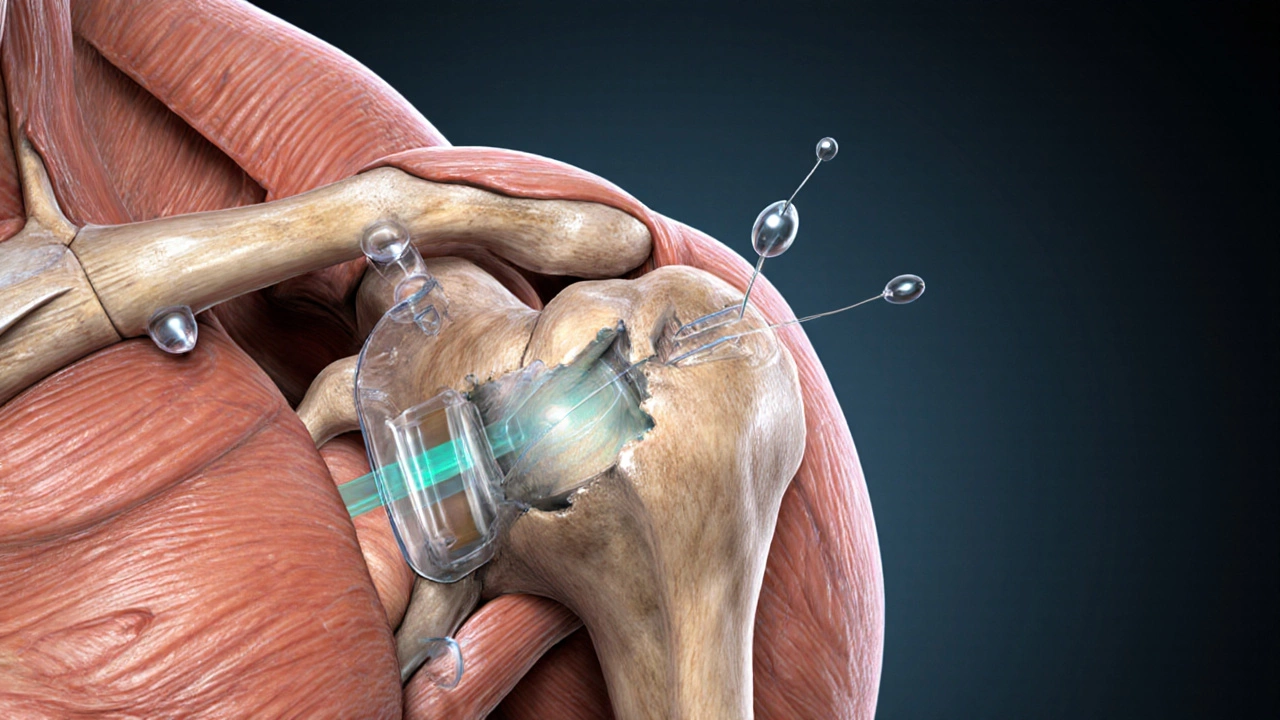
What Is a Rotator Cuff Repair?
Rotator Cuff Repair is a surgical procedure that re‑attaches torn shoulder tendons to the humerus, restoring strength and range of motion. The rotator cuff comprises four tendons - supraspinatus, infraspinatus, teres minor, and subscapularis - that hold the head of the humerus inside the shallow socket of the shoulder blade. When one or more of these tendons tear, patients experience sharp pain, especially at night, and a noticeable drop in lifting ability.
When Is Surgery Recommended?
- Full‑thickness tear confirmed by MRI or ultrasound.
- Persistent pain despite 3‑6 months of conservative treatment (physical therapy, NSAIDs, steroid injections).
- Young or active patients who need to return to overhead activities (e.g., athletes, manual laborers).
- Degenerative tears in older adults when the tendon retraction is significant and causes functional loss.
If any of these criteria match, an orthopedic surgeon will discuss repair options.
Surgical Techniques: Open vs. Arthroscopic
Two main approaches exist:
- Open Repair: A 4‑6 inch incision gives direct visual access to the torn tendon. It’s often used for massive, retracted tears because the surgeon can manipulate the tissue more freely.
- Arthroscopic Repair: Small (5‑10 mm) portals allow a camera and instruments to work inside the joint. Benefits include less postoperative pain, smaller scar, and faster early rehab. Most surgeons now prefer the arthroscopic method for standard‑size tears.
Both techniques use sutures or anchors to secure the tendon back to the bone, and many surgeons augment the repair with a biologic patch to promote healing.
Recovery Timeline and Rehabilitation
Recovery is a marathon, not a sprint. Here’s a typical path:
- Weeks 0‑2: Sling immobilization, passive range‑of‑motion exercises performed by a therapist.
- Weeks 3‑6: Transition to active assisted motion; light scapular strengthening.
- Weeks 7‑12: Begin resistance training, focusing on rotator cuff and deltoid muscles.
- Months 4‑6: Full activity resumption, sport‑specific drills for athletes.
Adherence to physical therapy dramatically influences the final outcome. Studies show that patients who complete a structured rehab program regain 80‑90% of pre‑injury strength, while those who skip therapy often suffer re‑tear rates of 20% or higher.
Outcomes, Success Rates, and Risks
Modern arthroscopic repairs boast a 90%‑95% success rate in restoring function and relieving pain. However, potential complications include:
- Stiffness or frozen shoulder.
- Infection (rare, 1‑2%).
- Anchor failure or tendon re‑tear, especially if rehab is rushed.
- Neurovascular injury (extremely uncommon).
Long‑term follow‑up studies reveal that most patients remain pain‑free and functional beyond ten years, provided they avoid heavy overhead loads without proper conditioning.

How Rotator Cuff Repair Stacks Up Against the Other Top Surgeries
When you compare the fifth‑ranked procedure with the four ahead of it, a few themes emerge:
- Invasiveness: Rotator cuff repair is less invasive than lumbar spinal fusion but more involved than a simple knee arthroscopy.
- Recovery Length: It sits in the middle - longer than hip/knee replacements (which have accelerated rehab protocols) but shorter than spinal fusion.
- Cost: At $15‑$20k, it’s cheaper than joint replacements and spinal fusion, yet pricier than outpatient arthroscopy.
- Patient Demographics: Overlap with joint replacement ages, but shoulder issues often affect active individuals who need a quick return to overhead work.
Understanding these trade‑offs helps patients and families decide whether to pursue surgery now or continue non‑operative care.
Choosing the Right Orthopedic Surgeon and Facility
Not all surgeons are equal. Look for:
- Board certification in orthopedic surgery with a fellowship in shoulder & elbow.
- Annual volume of at least 30‑40 rotator cuff repairs - higher volume correlates with better outcomes.
- Access to a dedicated shoulder rehab team.
- Transparent discussion of technique (open vs. arthroscopic) and implant choices.
Many top hospitals publish their surgeon-specific outcomes; don’t hesitate to request that data.
Post‑Surgery Tips to Maximize Healing
- Follow the sling schedule: Keep the arm supported as prescribed; premature movement can stretch the repair.
- Attend every PT session: Consistency beats intensity - small daily motions prevent scar tissue buildup.
- Manage pain wisely: Use prescribed NSAIDs and avoid opioid dependence; adequate pain control encourages active participation in rehab.
- Nutrition matters: Protein intake of 1.2‑1.5 g/kg body weight, plus vitamin C and zinc, supports tendon healing.
- Watch for red‑flag signs: Increasing redness, swelling, or fever may signal infection - call your surgeon immediately.
Frequently Asked Questions
How long does a rotator cuff repair surgery take?
Most arthroscopic repairs last 1.5‑2 hours, while open repairs can extend to 2.5‑3 hours depending on tear size.
Can a rotator cuff heal without surgery?
Partial, small tears often improve with a supervised PT program and activity modification, but full‑thickness tears in active adults usually need surgical fixation for long‑term strength.
What’s the difference between a tear and a tendinopathy?
A tear means a visible discontinuity of tendon fibers, while tendinopathy refers to degeneration or inflammation without a complete split.
Will insurance cover rotator cuff repair?
Most major insurers consider it medically necessary when conservative care fails, but prior authorization and documentation of functional loss are typically required.
When can I return to weight‑lifting after surgery?
Light resistance work can begin around 12‑16 weeks, but heavy lifting or overhead presses usually wait until 6 months, once strength tests show ≥80% of the non‑operative side.
Knowing that rotator cuff repair sits at the fifth spot helps set realistic expectations about volume, expertise, and recovery pathways. Whether you’re a patient, a family member, or a health‑care professional, understanding the procedure’s place in the orthopedic hierarchy guides better decisions and smoother outcomes.






