Joint & Muscle Pain Specialist Finder
This tool helps you determine which medical specialist is best suited for your joint or muscle pain symptoms. Based on the description in the article, answer the following questions to receive a recommendation.
1. Where do you feel the most pain?
2. Do you experience any of these symptoms?
3. What type of pain do you have?
4. How long have you been experiencing pain?
Dealing with nagging joint or muscle aches can feel like hitting a wall you can’t climb. The big question most people face is: who should actually see you for relief? Is it an joint pain doctor, a muscle‑focused therapist, or maybe a mix of both? Below we break down the main medical specialties that handle bone‑and‑muscle complaints, point out what each one does best, and give you a simple way to pick the right professional for your specific issue.
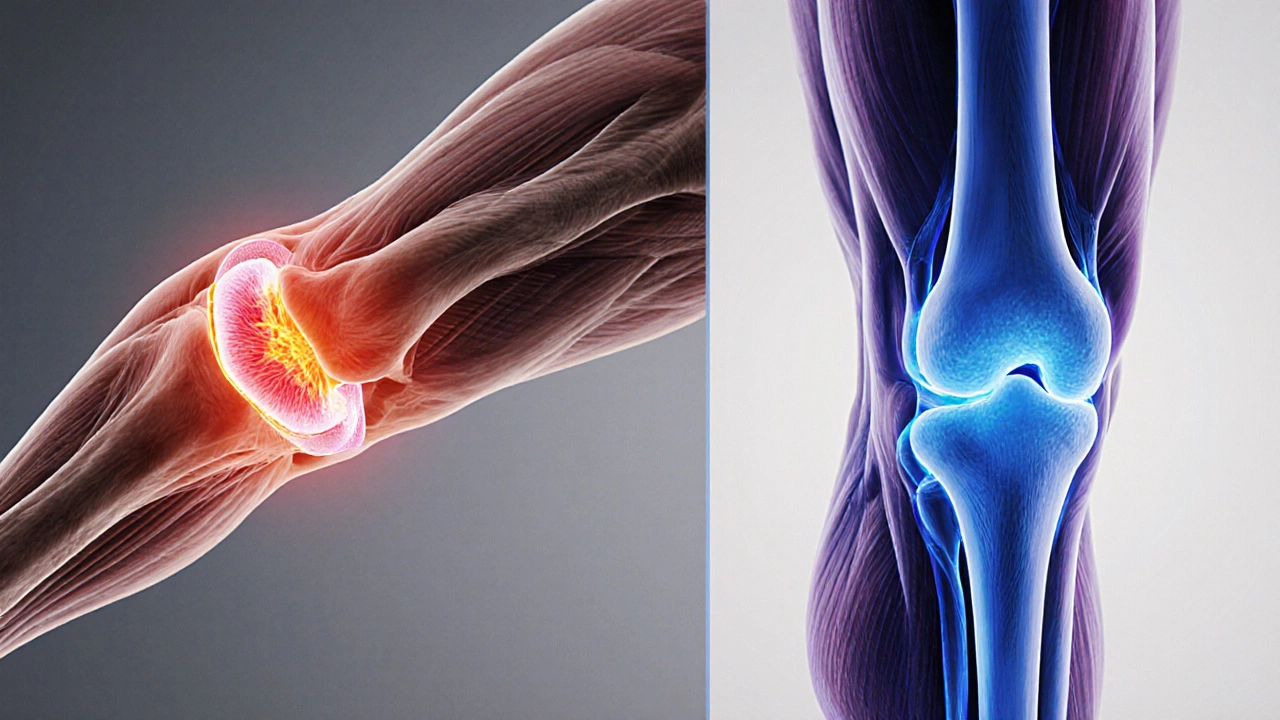
What’s the difference between joint pain and muscle pain?
Joint pain arises where two bones meet - think knees, hips, shoulders, wrists or elbows. It often involves cartilage, ligaments, the joint capsule, or the underlying bone itself. Common causes include osteoarthritis, rheumatoid arthritis, bursitis, meniscal tears, and gout.
Muscle pain (myalgia) usually stems from strained fibers, over‑use, inflammatory conditions, or nerve irritation that radiates into the muscle. Examples are muscle strains, fibromyalgia, myositis, and trigger‑point pain.
Even though the symptoms can overlap - you might feel a dull ache that seems to bounce between joint and muscle - the underlying pathology often dictates which specialist will provide the most targeted treatment.
Orthopedic Surgeon: The go‑to for structural joint problems
Orthopedic Surgeon is a medical doctor who specializes in diagnosing, treating, and preventing disorders of the musculoskeletal system, which includes bones, joints, ligaments, tendons, and muscles. They complete a 4‑year medical degree, a 5‑year orthopedic residency, and often a 1‑2‑year fellowship focused on joint reconstruction, sports injuries, or spine surgery. When you have clear structural damage - a torn meniscus, severe osteoarthritis, a fractured pelvis, or a dislocated shoulder - an orthopedic surgeon can evaluate whether surgery, joint replacement, or minimally invasive procedures are needed.
Typical conditions they manage:
- Advanced osteoarthritis of the knee or hip
- Ligament tears (ACL, MCL, rotator cuff)
- Fractures that require internal fixation
- Spinal stenosis and vertebral compression fractures
Key treatment tools include arthroscopy, joint replacement, external fixation devices, and targeted rehabilitation plans.
Rheumatologist: The specialist for inflammatory joint and muscle disease
Rheumatologist is a physician who focuses on autoimmune and inflammatory disorders that affect joints, muscles, and connective tissue. After medical school they complete a 3‑year internal medicine residency followed by a 2‑year rheumatology fellowship. If your pain is linked to systemic inflammation - such as rheumatoid arthritis, lupus, gout, or polymyalgia rheumatica - a rheumatologist can order specific blood tests, imaging, and prescribe disease‑modifying drugs.
Typical conditions they manage:
- Rheumatoid arthritis
- Psoriatic arthritis
- Gout and pseudogout
- Systemic lupus erythematosus (musculoskeletal manifestations)
- Fibromyalgia (muscle‑wide pain syndrome)
Treatment often involves DMARDs (disease‑modifying anti‑rheumatic drugs), biologics, lifestyle counseling, and coordinated physical therapy.
Physiatrist (Physical Medicine & Rehabilitation Doctor): Bridging the gap
Physiatrist is a physician trained in physical medicine and rehabilitation (PM&R). Their focus is restoring function after injury or chronic disease without resorting to surgery. Training includes a 4‑year medical degree, a 4‑year residency in PM&R, and often a fellowship in sports medicine, pain management, or spinal disorders. They excel when you need a comprehensive, non‑surgical plan that combines injections, therapeutic exercises, and assistive devices.
Typical scenarios:
- Chronic low‑back pain with mixed joint and muscle components
- Post‑operative rehab after joint surgery
- Complex regional pain syndrome
- Neuromuscular weakness affecting joint stability
Sports Medicine Physician: For active lifestyles
Sports Medicine Physician is a doctor who treats injuries related to exercise and athletics. They may come from an orthopedic or primary‑care background and usually finish a 1‑year sports‑medicine fellowship. If you’re an athlete (amateur or pro) dealing with tendonitis, labral tears, or stress fractures, this specialist tailors rehab to get you back in the game quickly.
Typical conditions they manage:
- Patellar tendonitis (jumper’s knee)
- Achilles tendinopathy
- Rotator cuff tendinitis
- Stress fractures of the tibia or metatarsals
- Muscle strains from over‑use

Pain Management Specialist: When pain dominates daily life
Pain Management Specialist is a physician, often an anesthesiologist or physiatrist, who focuses on chronic pain control. Their toolbox includes nerve blocks, epidural steroid injections, radiofrequency ablation, and prescription‑monitoring programs. If your joint or muscle pain persists despite conventional care, they can assess whether interventional therapies or multimodal medication plans are appropriate.
Family Physician: The first point of contact
Family Physician provides comprehensive primary care for patients of all ages. With a broad training base, they can evaluate mild joint or muscle aches, order basic imaging, and refer you to a specialist when red flags appear. For many with occasional soreness, a family doctor can start you on NSAIDs, basic physiotherapy, and lifestyle advice before escalating care.
Comparison of specialties
| Specialty | Primary Focus | Typical Conditions | Usual Treatments | When to See |
|---|---|---|---|---|
| Orthopedic Surgeon | Structural bone & joint issues | Severe osteoarthritis, fractures, ligament tears | Surgery, arthroscopy, joint replacement | Persistent mechanical pain, instability, imaging shows damage |
| Rheumatologist | Inflammatory & autoimmune disorders | Rheumatoid arthritis, gout, lupus, fibromyalgia | DMARDs, biologics, lab monitoring, rehab | Swelling, morning stiffness, systemic symptoms |
| Physiatrist | Rehabilitation & functional recovery | Chronic back pain, post‑surgery rehab, neuropathic pain | Injection therapy, exercise prescription, assistive devices | Pain limits daily function, non‑surgical approach preferred |
| Sports Medicine Physician | Activity‑related injuries | Tendonitis, stress fractures, muscle strains | Targeted rehab, bracing, minimally invasive procedures | Active individual, wants quick return to sport |
| Pain Management Specialist | Chronic pain control | Failed conservative therapy, neuropathic pain | nerve blocks, medication plans, neuromodulation | Pain dominates life despite other treatments |
| Family Physician | General primary care | Mild strains, early arthritis, nonspecific aches | NSAIDs, basic PT referral, lifestyle counseling | First point of contact, needs screening |
How to choose the right doctor for your situation
- Identify the dominant symptom. Is the pain sharp and localized to a joint, or is it a diffuse ache that worsens with activity?
- Look for red‑flag signs. Swelling, fever, sudden loss of motion, or numbness require urgent specialist evaluation.
- Match the symptom to specialty. Structural damage → Orthopedic Surgeon; inflammation → Rheumatologist; ongoing functional limitation → Physiatrist; sport‑related injury → Sports Medicine Physician.
- Check credentials and experience. Look for board certification, fellowship training, and volume of relevant cases (e.g., >150 knee replacements per year).
- Consider logistics. Proximity, insurance coverage, and appointment wait‑times can affect adherence.
What to expect at your first appointment
Regardless of the specialist, the initial visit usually follows a predictable pattern:
- Medical history. Detailed questions about pain onset, aggravating/relieving factors, past injuries, and family history of arthritis.
- Physical examination. Range‑of‑motion testing, palpation of joints and muscles, gait analysis, and specific stress tests.
- Imaging or labs. X‑rays, MRI, or blood tests (CRP, ESR, rheumatoid factor) may be ordered on the spot or scheduled later.
- Discussion of treatment plan. The doctor will outline options ranging from watchful waiting to medication, injections, therapy, or surgery.
Bring a list of current medications, any recent imaging reports, and notes on what makes your pain better or worse. Clear communication helps the doctor pinpoint the cause faster.
Red flags that need immediate medical attention
While most joint and muscle pain is manageable, certain signs suggest a serious underlying problem:
- Sudden severe pain after a fall or twist
- Visible deformity or joint instability
- Fever, chills, or unexplained weight loss
- Progressive weakness or numbness affecting daily activities
- Rapid swelling that does not improve with rest or ice
If any of these appear, head to the emergency department or call your primary care doctor right away.
Key takeaways
- Joint‑specific structural problems usually need an Orthopedic Surgeon.
- Inflammatory or autoimmune‑driven pain is best managed by a Rheumatologist.
- When function and rehabilitation are the priority, consider a Physiatrist or Sports Medicine Physician.
- Chronic, refractory pain may benefit from a Pain Management Specialist.
- Start with a Family Physician for screening, basic care, and referrals.
Frequently Asked Questions
Do I need an MRI before seeing a specialist?
Often the first doctor will order basic X‑rays. If those don’t explain the pain, or if the specialist suspects soft‑tissue injury, an MRI is usually the next step.
Can a physiotherapist treat joint pain without a doctor?
Physiotherapists can help with pain relief and mobility, but they cannot prescribe medication or perform surgery. They should work under a doctor’s referral for best outcomes.
How long does recovery take after knee replacement?
Most patients regain basic walking ability within 4‑6 weeks, but full strength and high‑impact activities may take 4‑6 months, guided by a physiatrist‑led rehab program.
Is joint pain always a sign of arthritis?
No. Joint pain can stem from injuries, bursitis, meniscal tears, or temporary overuse. Arthritis is just one of many possible causes.
When should I consider seeing a pain management specialist?
If pain persists for more than 3‑6 months despite physical therapy, NSAIDs, and specialist referral, it’s time to explore interventional options with a pain management doctor.