Rheumatologist: What They Do and When You Need One
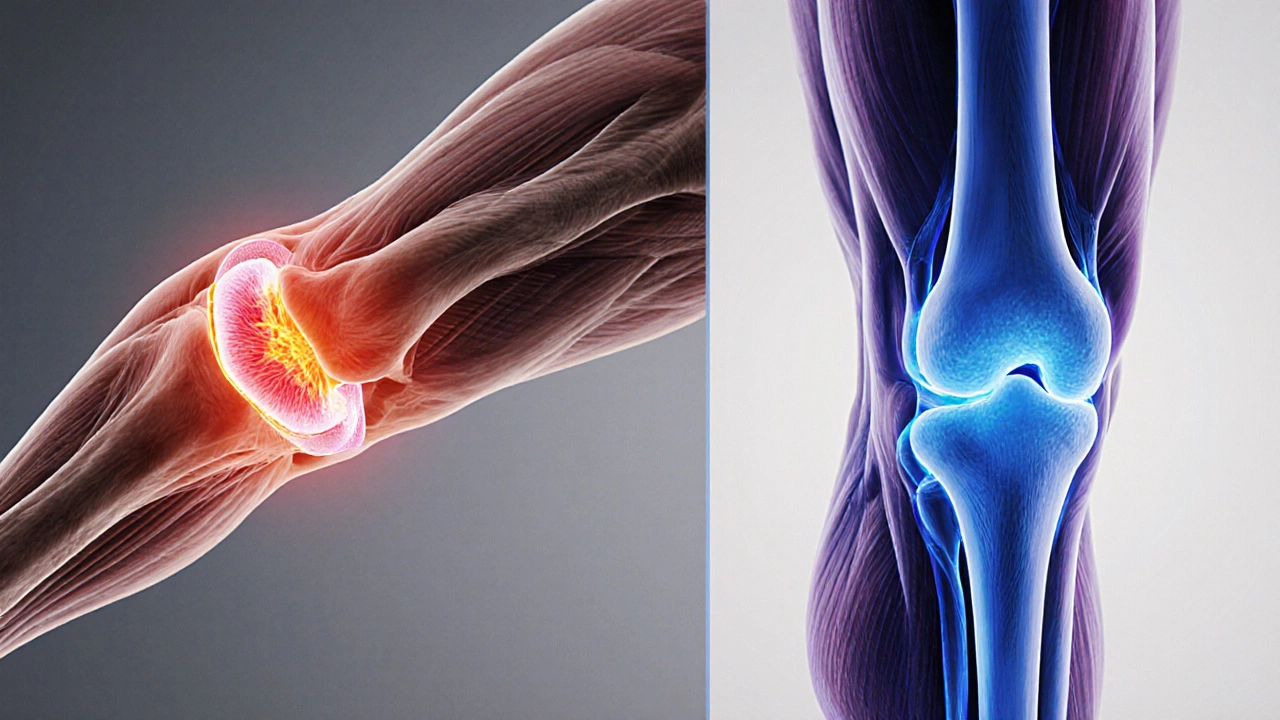
A rheumatologist, a doctor who diagnoses and treats diseases affecting the joints, muscles, and immune system. Also known as a joint specialist, they focus on conditions like arthritis, lupus, and other autoimmune disorders that don’t show up on regular X-rays but cause real, lasting pain. Unlike orthopedic surgeons who fix broken bones or replace joints, rheumatologists work behind the scenes to stop the body from attacking itself.
If you’ve had swollen knees for months, wake up stiff every morning, or get rashes along with joint pain, you’re not just "getting older"—you might have an autoimmune disease, a condition where the immune system mistakenly targets healthy tissue. Conditions like rheumatoid arthritis, psoriatic arthritis, or ankylosing spondylitis don’t go away on their own. Left untreated, they can destroy joints, damage organs, and leave you unable to walk, grip a cup, or even button a shirt. A rheumatologist uses blood tests, imaging, and symptom patterns to spot these hidden problems early—before the damage becomes permanent.
They also treat rheumatic conditions, a broad group of over 100 disorders that cause inflammation in connective tissues, including fibromyalgia, gout, and vasculitis. These aren’t just "aches and pains." Gout can turn a big toe into a burning hot lump. Lupus can make your kidneys fail. Fibromyalgia can leave you exhausted even after sleeping all night. A general doctor might miss these signs. A rheumatologist knows what to look for.
You don’t need a referral to see one if you’re suspicious—but most people are sent by their primary care provider after routine tests come back abnormal. High CRP or ESR levels, positive rheumatoid factor, or unexplained fatigue often trigger the referral. If you’ve tried painkillers, physical therapy, or rest and nothing sticks, it’s time to ask about a rheumatologist. They don’t just prescribe pills—they create long-term plans that include diet, exercise, and monitoring to keep you moving.
The good news? Many of these conditions can be managed well today. New medications can stop joint damage before it starts. Early diagnosis means you can live a full life without constant pain. The bad news? Too many people wait too long. They think joint pain is normal. It’s not. If your body is sending you signals—swelling, stiffness, unexplained fever, or numbness—it’s worth getting checked by someone who specializes in these hidden battles.
Below, you’ll find real-life guides on blood tests, supplements, and recovery that connect to what rheumatologists see every day—from how liver health affects arthritis meds to why some herbal supplements can make autoimmune symptoms worse. These aren’t random articles. They’re the practical pieces you need when you’re navigating life with a chronic joint or immune condition.
Which Doctor Treats Joint and Muscle Pain Best?
Learn which doctors treat joint and muscle pain, compare specialties, and get a clear guide to choosing the right professional for lasting relief.