Daily Functioning Assessment
This assessment helps you understand how mental health conditions might affect daily functioning. Based on the article's definition of disabling mental illnesses, you'll rate your ability to perform essential activities.
Your Assessment Results
What Your Score Means
Your assessment suggests minimal impact on daily functioning. This doesn't mean there aren't challenges—mental health exists on a spectrum—but it indicates you're currently able to maintain most essential activities.
Key Takeaways from the Article
According to the article, mental illnesses become "disabling" when they significantly impact your ability to work, manage daily tasks, or maintain relationships. The assessment measures exactly these critical areas.
Remember: Even with low scores, it's important to be aware of warning signs. The article emphasizes that many conditions are treatable with appropriate support.
If you're experiencing persistent difficulties, please consider reaching out to a professional. You're not alone.
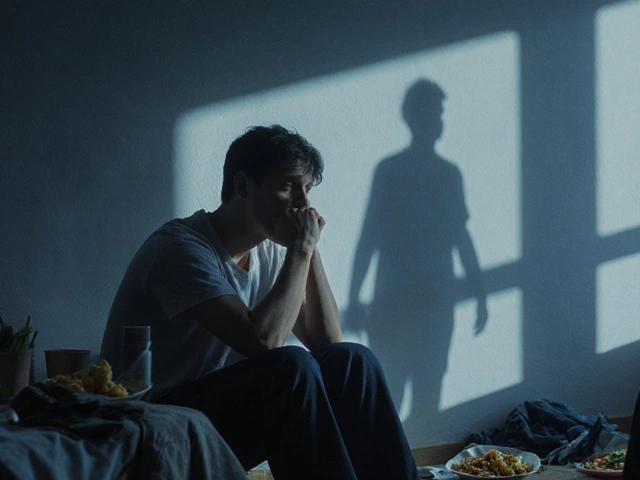
When people talk about mental illness, they often think of sadness, stress, or anxiety. But some mental illnesses don’t just make life harder-they break your ability to work, care for yourself, or even connect with others. These aren’t just "bad days." They’re conditions that rewrite how your brain functions, often for years, sometimes for life.
What Makes a Mental Illness "Disabling"?
A disabling mental illness isn’t defined by how loud the symptoms are, but by how deeply they cut into daily life. If you can’t hold a job, pay bills, cook a meal, or leave the house without panic, that’s disability. The World Health Organization ranks mental disorders among the top causes of disability worldwide. In India alone, over 7% of the population lives with a severe mental health condition that limits their independence.
Disability here means: missing work for weeks, needing help with basic tasks, losing relationships, or being unable to manage medications without support. It’s not about being "weak." It’s about brain chemistry, trauma, genetics, and environment colliding in ways that no amount of willpower can fix.
1. Schizophrenia
Schizophrenia doesn’t mean multiple personalities. It means losing touch with reality. People with this condition hear voices that aren’t there, believe things that are clearly false, or withdraw so completely they stop speaking. Hallucinations and delusions can be terrifying-not just for the person, but for everyone around them.
Many can’t hold jobs because their thoughts jump uncontrollably. Others can’t bathe or eat regularly because they don’t believe they need to. About 20% of people with schizophrenia attempt suicide at least once. Medication helps, but it doesn’t cure. Long-term support, therapy, and community care are essential. Without them, homelessness and incarceration become common outcomes.
2. Severe Major Depressive Disorder
Depression isn’t just feeling down. Severe depression is a full-body shutdown. People describe it as being trapped in concrete. They sleep 16 hours a day-or not at all. They lose weight because food tastes like ash. They cry for no reason, or stop crying because they’re too numb to feel anything.
It’s not about laziness. Brain scans show reduced activity in areas that control motivation and pleasure. In India, over 50 million people live with depression. Many never seek help because of stigma. Those who do often wait years. By then, they’ve lost jobs, relationships, and sometimes, hope. Electroconvulsive therapy (ECT) and intensive psychotherapy can bring people back-but only if they get help in time.
3. Bipolar Disorder (Type I)
Bipolar isn’t just mood swings. Type I means extreme highs-manic episodes where people spend thousands, sleep for two hours, or believe they’re famous or divine-followed by crushing lows that can last months. During mania, judgment vanishes. People quit jobs, gamble away savings, or get into dangerous relationships.
The risk of suicide is 15 to 20 times higher than in the general population. Many go undiagnosed for years because the highs feel good. By the time they seek help, they’ve lost everything. Lithium and mood stabilizers work-but only if taken daily. Missing doses can trigger relapse. This isn’t something you can "snap out of." It’s a lifelong condition that demands structure, medication, and constant monitoring.
4. Obsessive-Compulsive Disorder (OCD)
OCD isn’t about being neat. It’s about being trapped in your own mind. Someone might wash their hands until they bleed because they fear germs. Another might check the stove 50 times a night, terrified they’ll burn down the house. Thoughts spiral. Rituals multiply. Time vanishes.
In severe cases, people spend 6 to 10 hours a day on compulsions. They miss work. They stop seeing friends. Some can’t leave their homes because the outside world feels too dangerous. Exposure and Response Prevention (ERP) therapy is the gold standard-but access is limited in India. Medication helps, but it’s not a cure. The struggle is invisible, which makes it harder to get support.

5. Post-Traumatic Stress Disorder (PTSD)
PTSD doesn’t only affect soldiers. It hits survivors of domestic violence, sexual assault, accidents, natural disasters, and even witnessing trauma. The brain gets stuck in fight-or-flight mode. Loud noises, smells, or even a certain time of day can trigger panic attacks, flashbacks, or dissociation.
People with PTSD often avoid people, places, or activities that remind them of the trauma. They sleep poorly. They’re easily startled. Many turn to alcohol or drugs to numb the pain. In India, where trauma care is scarce, PTSD can become a life sentence. Trauma-focused CBT and EMDR therapy can help-but only if you can find a trained therapist. Most can’t.
6. Borderline Personality Disorder (BPD)
BPD isn’t about being "dramatic." It’s about emotional instability so intense it destroys relationships and self-image. People with BPD feel abandonment like a physical threat. They may lash out, self-harm, or attempt suicide after a minor argument. Their moods shift in minutes. One day they love you; the next, they hate you.
Many grow up with childhood trauma. They struggle to hold jobs because of emotional outbursts. They lose friends because no one knows how to respond. Dialectical Behavior Therapy (DBT) is the only proven treatment. It teaches emotional regulation, but it’s hard to access. In India, few clinics offer it. Without treatment, BPD leads to chronic crisis, hospitalizations, and isolation.
7. Severe Anxiety Disorders (Generalized, Social, Panic)
Anxiety isn’t just being nervous. Severe anxiety means your body is in constant alarm. Your heart races without reason. You feel like you’re choking. You avoid elevators, crowds, or even phone calls. Social anxiety isn’t shyness-it’s terror of being judged. Panic attacks can feel like heart attacks.
People with severe anxiety often quit jobs, drop out of school, or become housebound. They know their fears are irrational, but logic doesn’t work. SSRIs and CBT help, but many avoid treatment because they think they should just "get over it." In rural India, anxiety is dismissed as "stress." It’s not. It’s a neurological condition that rewires the brain’s fear response.
8. Eating Disorders (Anorexia, Bulimia, Binge Eating)
Eating disorders are the deadliest mental illnesses. Anorexia kills more people than any other psychiatric condition. People starve themselves because they see fat in the mirror-even when they’re skeletal. Others binge and purge, or eat nonstop to numb emotional pain.
The body breaks down: bones weaken, hearts fail, organs shut down. Recovery takes years. Many relapse. Family-based therapy works for teens. Adults need intensive outpatient or residential programs. In India, eating disorders are rarely diagnosed. Doctors see weight loss as a success. Families see it as discipline. No one sees the mental torture behind it.

9. Autism Spectrum Disorder (ASD) with Severe Impairment
Not everyone with autism is high-functioning. For some, communication is nearly impossible. They may never speak. They scream when overwhelmed. They rock for hours. They can’t dress themselves or use the toilet without help. Sensory overload-light, sound, touch-can trigger meltdowns.
Many live in institutions because families can’t manage the care. In India, early diagnosis is rare. Therapy is expensive and scarce. Adults with severe ASD often have no access to jobs, housing, or social services. They’re invisible. Their needs are ignored. Support systems barely exist.
10. Dementia (Alzheimer’s and Other Types)
Dementia isn’t just forgetting names. It’s losing your identity. People forget their children’s faces. They wander off and can’t find home. They get angry over nothing. They forget how to eat, bathe, or walk. Alzheimer’s is the most common-but vascular dementia, Lewy body, and frontotemporal dementia are just as disabling.
India has over 4 million people with dementia. That number will double by 2030. Families struggle to care for them. No national support system exists. Many are chained to beds or locked in rooms because no one knows how to help. Medications slow decline-but don’t stop it. Compassionate care is the only real treatment. And it’s in short supply.
Why These Illnesses Are So Hard to Treat
These conditions don’t show up on X-rays. No blood test confirms schizophrenia or OCD. Diagnosis relies on observation, history, and symptoms. That’s why they’re underdiagnosed, especially in rural areas.
Medication helps-but doesn’t fix everything. Therapy is essential, but trained professionals are scarce. In India, there’s less than one psychiatrist per 100,000 people. Insurance rarely covers mental health. Stigma silences families. People suffer alone.
Recovery isn’t linear. Relapse is common. Progress is measured in small wins: showering, eating one meal, making a phone call. But those wins matter.
What Can Be Done?
Change starts with recognition. These aren’t "personal failures." They’re medical conditions. We need:
- More community mental health centers
- Training for primary care doctors to spot early signs
- Insurance that covers therapy and medication
- Public campaigns to reduce stigma
- Support groups for families
And most of all-we need to stop pretending these illnesses aren’t real. They are. And they’re disabling millions of lives, quietly, every day.
Are these mental illnesses curable?
Most of these conditions aren’t "cured" like an infection. But they can be managed. With the right treatment-medication, therapy, and support-many people live full, productive lives. Recovery means learning to live with the illness, not being free of it.
Can someone with schizophrenia work?
Yes, many do. With stable medication, structured routines, and workplace accommodations, people with schizophrenia can hold jobs. Some work remotely, part-time, or in supportive environments. The key is consistency and reducing stress triggers. It’s not easy, but it’s possible.
Why is mental illness so stigmatized in India?
Cultural beliefs often link mental illness to weakness, bad karma, or spiritual possession. Families hide it to avoid shame. Many believe prayer or Ayurveda alone can fix it. This delays real treatment. Education and open conversations are slowly changing this-but progress is slow.
What’s the difference between depression and sadness?
Sadness comes and goes. Depression lasts weeks or months. It doesn’t lift with good news or a vacation. It drains energy, sleep, appetite, and motivation. It’s not about what’s happening outside-it’s about how your brain processes the world. Sadness is a feeling. Depression is a disease.
Can children have these disorders too?
Yes. Depression, anxiety, OCD, and even early signs of schizophrenia can appear in childhood. Autism and eating disorders often show up in teens. But kids rarely get diagnosed because symptoms are mistaken for "bad behavior" or "phase." Early intervention changes outcomes dramatically.
Are these illnesses genetic?
Genetics play a role, but they’re not the whole story. Schizophrenia, bipolar disorder, and autism have strong hereditary links. But trauma, stress, infections, and environment can trigger them-even in people with no family history. It’s a mix of biology and life experience.
How do I help someone with a severe mental illness?
Don’t tell them to "snap out of it." Listen without judgment. Help them find a qualified therapist. Offer to go with them to appointments. Help with daily tasks if they’re overwhelmed. Be patient. Recovery takes time. Your presence alone can be lifesaving.