GLP-1 Safety: What You Need to Know About Weight-Loss Drugs Like Ozempic and Zepbound
When you hear GLP-1, a class of hormones that help regulate blood sugar and appetite, often used in diabetes and weight-loss medications. Also known as GLP-1 receptor agonists, these drugs are changing how doctors treat obesity — but they’re not risk-free. Drugs like Ozempic, Wegovy, and Zepbound work by slowing digestion, reducing hunger, and helping your body use insulin better. They’ve helped millions lose weight, but they’ve also sparked real concerns about side effects, long-term safety, and who should avoid them.
The most common issue? Nausea. Up to half of users feel sick, especially when starting. That’s not just discomfort — it can mean vomiting, loss of appetite, or even dehydration. Less common but serious risks include pancreatitis, gallbladder disease, and rare cases of thyroid tumors seen in animal studies. The FDA hasn’t confirmed these tumors happen in humans, but it’s still a warning flag. People with a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia should not use these drugs. And while they’re often marketed as "magic pills," they don’t work without lifestyle changes. If you keep eating the same high-sugar, high-fat meals, the drug won’t save you.
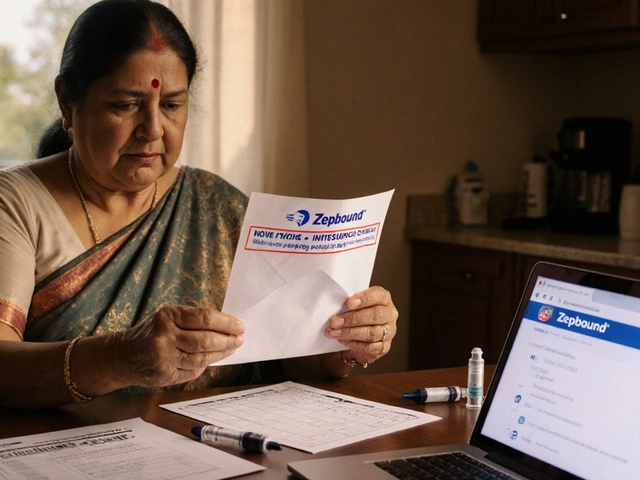
Another layer is cost and access. Insurance often denies coverage for Zepbound, a newer GLP-1 medication approved for weight loss, similar to semaglutide but with added ingredients. Even when approved, monthly prices can hit $1,000 or more. And while clinics push these drugs hard, many don’t follow up with patients on monitoring — no blood tests, no check-ins on mood or digestion. That’s dangerous. These aren’t OTC supplements. They’re prescription medications that need oversight.
What about the long haul? We don’t have 10-year data yet. Most studies run 1-2 years. We know people regain weight if they stop. We know some develop muscle loss or nutrient deficiencies because they eat too little. And we’re only now seeing reports of mental health changes — depression, anxiety, or suicidal thoughts — in a small number of users. No one’s saying these drugs are unsafe for everyone. But safety isn’t just about avoiding a hospital visit. It’s about living well, not just losing weight.
Below, you’ll find real, no-fluff breakdowns of what these drugs actually do to your body, who should avoid them, what side effects are most common, and how clinics are handling (or ignoring) the risks. Whether you’re considering one of these drugs, already using one, or just confused by the hype — this collection gives you the facts without the marketing.
Safest Diabetic Pill: What You Need to Know
Learn which diabetes pills are safest by comparing hypoglycemia risk, kidney and heart impact, and real‑world side‑effects to pick the right medication for you.